Difference Between MRSA and MSSA

Introduction
Methicillin is an antibiotic used to treat bacterial infections. More specifically, it is classed as a narrow-spectrum β-lactam antibiotic. When it comes to bacteria, methicillin is used to treat a strain called Staphylococcus aureus. This bacterium is associated with skin, blood infection and pneumonia in the lungs.
MRSA and MSSA and two acronyms for a larger description of the interactions between Staphylococcus aureus bacteria and methicillin β-lactam antibiotic treatments. Both equally as important to understand when it comes to the treatment of infection!

Definition and Pathophysiology
MRSA
MRSA is the acronym for “methicillin-resistant Staphylococcus aureus”. It specifically refers to strains of Staphylococcus aureus bacteria that have become resistant (or immune) to a variety of β-lactam antibiotic treatments.
These resistant strains are gram-positive bacteria. They usually grow to become resistant over longer periods of time. During this developing resistance, there is internal gene activity and types of natural selection which help them become increasingly immune to the antibiotic treatments.
MSSA
MSSA is the acronym for “methicillin-sensitive Staphylococcus aureus”. MSSA specifically refers to the strains of Staphylococcus aureus bacteria that are susceptible to β-lactam antibiotic treatments.
The susceptibility to β-lactam antibiotic treatments means that the Staphylococcus aureus bacteria related conditions are sensitive to treatment and thus, easily treatable.
Clinical Presentation & Behaviour of Bacterial Infection
Infections associated with MRSA and MSSA usually present as:
- Infections of the skin (such as boils or serious conditions like necrotizing fasciitis)
- Pneumonia of the lungs
- Bacterial infections of the heart
- Infections in surgical sites and around medical devices
- Infections of the bones and joints
Where MSSA goes on to heal and responds well to antibiotics, MRSA shows progressive infections including infected areas being warm to the touch, increased deepening and production of pus, and progression into a system fever and systematic shock.
Blood tests usually confirm the presence of Staphylococcus aureus and worsening progression indicate resistance. As confirmation, lab analysis will confirm the presence of MRSA.
Risk Factors
Risk factors for acquiring methicillin-resistant Staphylococcus aureus can be hospital related or community related. These risk factors include:
- Hospital stays (especially with a weak immune system)
- Invasive medical devices (such as drips and catheters)
- Staying in long-term care facilities (such as nursing homes)
- Contact sports with skin-to-skin contact
- Overcrowded and unsanitary environments (including jails, army camps, etc.)
- HIV infections
- Injected drug abuse
- Higher prevalence in sexual activity between male gender groups
The risk factors for acquiring methicillin-sensitive Staphylococcus aureus include:
- Skin-to-skin contact
- Contact with surfaces and items which have been contaminated with Staphylococcus aureus
- Sharing of personal items that come into contact with the skin cells (such as towels, razors, and sports equipment).
Treatment
Treating MRSA is challenging, as many antibiotics are no longer effective against the bacterial infection. Depending on the type of infection, alternative antibiotics can potentially be effective. Treatment of MSSA however, is more straightforward and treatment is effective.
The following infections can be treated with the therapy indicated:
MRSA
Vancomycin: complex skin infections, bacteraemia, catheter infections, bone infections and pneumonia.
Clindamycin and linezolid: simple skin infections and pneumonia
MSSA
Cephalexin: simple skin infections
Nafcillin: all other infections
When it comes to MRSA, the chance of severe complications is quite high. The bacterial infection can become so resistant that limb amputation is often necessary and in some instances, the patient will not be able to fight off the infection thus resulting in death.
Prevention
MRSA infections can be prevented by sustaining good personal hygiene, covering skin lacerations, avoiding the sharing of personal items, removing feminine products every 4-8 hours, and getting early treatment if you suspect an infection.
In facilities, good hygiene, covering up of hands and surfaces, and regular sterilization can prevent the occurrence of MRSA.
MSSA infections can be prevented by good personal hygiene, covering skin lacerations, avoiding the sharing of personal items, and getting early treatment if you suspect an infection.
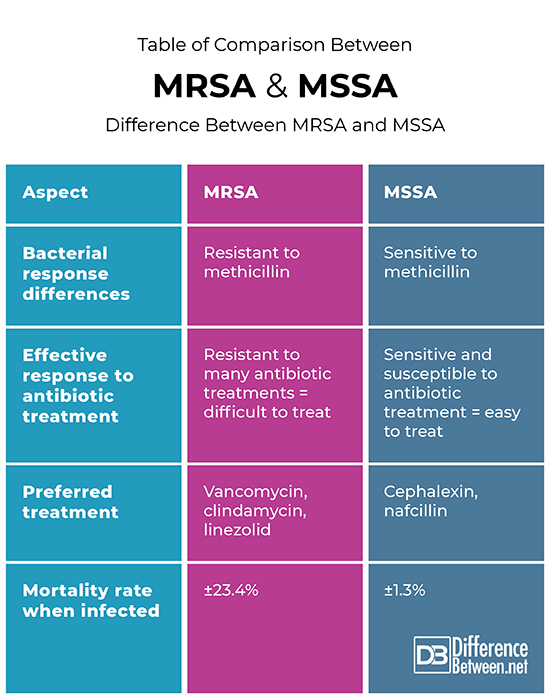
Table of comparison between MRSA and MSSA
Summary
MRSA and MSSA are both infections by the Staphylococcus aureus bacteria. MRSA is resistant to β-lactam antibiotic treatments, where MSSA is sensitive to these treatments. Both of these infections can be picked up when coming into direct contact with skin of another person, sharing personal items and touching contaminated products or surfaces. MRSA however, is also acquired in hospital settings, unhygienic facilities, unsanitary illicit drug practices and as post-operative complications.
In terms of treatment, MSSA can be easily treated with nafcillin and cephalexin, where MRSA can possibly be treated with vancomycin, clindamycin and linezolid. Unfortunately, the high level of resistance in certain MRSA infections may render treatment ineffective and result in long-term health implications, possible amputation and even death.
FAQ
Can MSSA turn into MRSA?
MSSA and MRSA are both conditions of the same bacteria, namely Staphylococcus aureus. The only difference between the two is their response to antibiotics. An MRSA strain of bacteria is a separate strain that is picked up in certain conditions. If you are infected with MSSA you will not have a bacterial mutation into MRSA from the same infection.
What do MSSA and MRSA mean?
MSSA is the acronym for “methicillin-sensitive Staphylococcus aureus”. MSSA specifically refers to the strains of Staphylococcus aureus bacteria that are susceptible to β-lactam antibiotic treatments.
The susceptibility to β-lactam antibiotic treatments means that the Staphylococcus aureus bacteria related conditions are sensitive to treatment and thus, easily treatable.
MRSA is the acronym for “methicillin-resistant Staphylococcus aureus”. It specifically refers to strains of Staphylococcus aureus bacteria that have become resistant (or immune) to a variety of β-lactam antibiotic treatments.
How does a person get MSSA?
The risk factors for getting infected with methicillin-sensitive Staphylococcus aureus include skin-to-skin contact, contact with surfaces and items which have been contaminated with Staphylococcus aureus, and the sharing of personal items that come into contact with the skin cells (such as towels, razors, and sports equipment).
- Difference Between a Cochlear Implant and Normal Hearing - October 4, 2022
- Difference Between Obstructive and Restrictive Spirometry - September 11, 2022
- The Difference Between White Box and Black Box Testing - September 11, 2022
Search DifferenceBetween.net :
Leave a Response
References :
[0]Bamberger, David and Boyd, Sarah. “Management of Staphylococcus aureus Infections”. American Family Physician, vol. 72, no. 12, 2005, pp. 2474-2481
[1]Blot, Stihn., Vandewoude, Koenraad and Hoste, Eric. “Outcome and Attributable Mortality in Critically Ill Patients With Bateremia Involving Methicillin-Suscetible and Methicillin-Resistant Staphylococcus aures”. Archives of Internal Medicine, vol. 162, no. 19, 2002, pp. 2229-2235
[2]Centres for Disease Control and Prevention. Methicillin-resistant Staphylococcus aureus (MRSA). https://www.cdc.gov/mrsa/community/index.html
