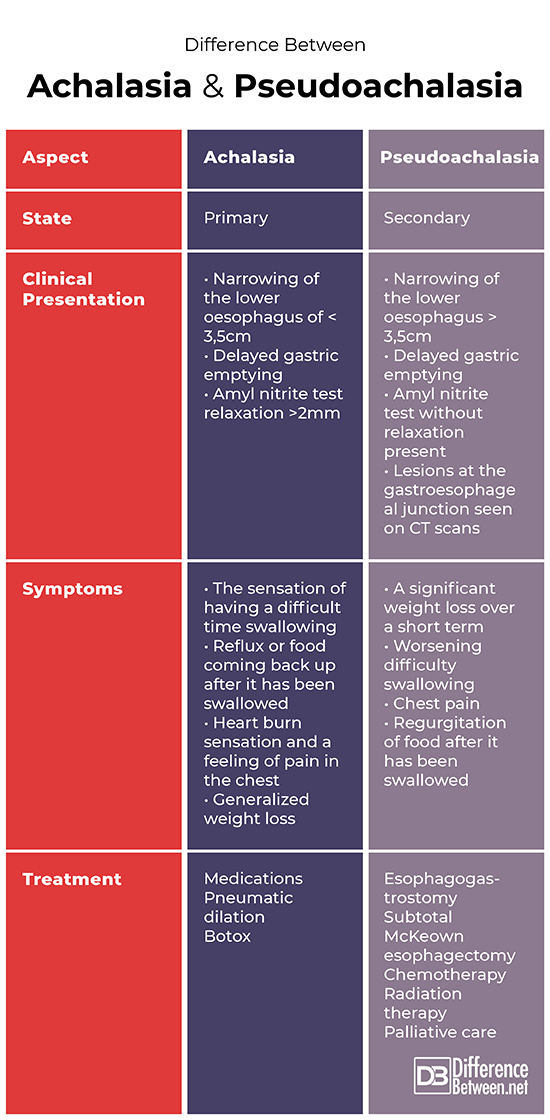
Difference Between Achalasia and Pseudoachalasia
Introduction
Achalasia and pseudoachalasia are both conditions involving oesophageal motility disorder. Both conditions are diagnosed using medical imaging and scoping procedures. Achalasia is a primary type of condition and pseudoachalasia is secondary.
Although similar, the causes and treatment plans differ significantly.
This article will help explore the ins and outs of achalasia and pseudoachalasia.
Definition and Causes
Achalasia
Achalasia is defined as an oesophageal motility disorder and is classified being of primary type.
It is generally characterized by the absence of muscle contractions known as oesophageal peristalsis and an improper relaxation of the lower oesophageal sphincter (the muscle at the bottom of the oesophagus) in relation to swallowing motions. In fact, the lower oesophageal sphincter muscle is considered by physicians to be in a hyper tensed/contracted state in roughly 50 % of the patients suffering from this condition. This abnormal function can lead to a blockage further down at the gastroesophageal junction.
The pinpoint causes of achalasia are unknown. It is suspected that a loss of nerve cells in the oesophagus are what causes this condition. Other causal factors such as viruses and autoimmune diseases are also suspected by research specialists in the field.
Pseudoachalasia
Pseudoachalasia is a type of secondary achalasia that most often occurs in adults over the age of 50 years old.
It is defined as a secondary achalasia caused by malignant tumours or by a chronic medical disease. This condition is difficult and challenging to diagnose in the early phases. In fact, roughly 25% of cases present as false negatives during tests and biopsies.
In cases where causes are benign, they can include tumours classified as benign mesenchymal tumours, stages of peripheral neuropathy, and the condition of secondary amyloidosis. Other lesser seen benign causes are sarcoidosis, aortic aneurysms, surgeries, juvenile Sjogren syndrome and other types of benign tumours.
Clinical Presentation and Diagnosis
Achalasia
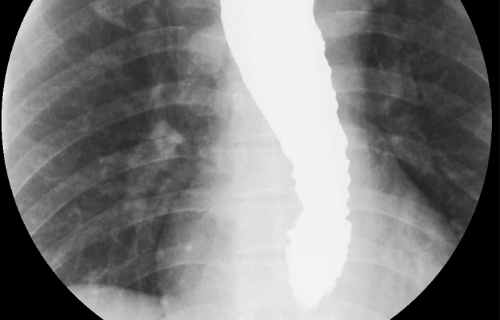
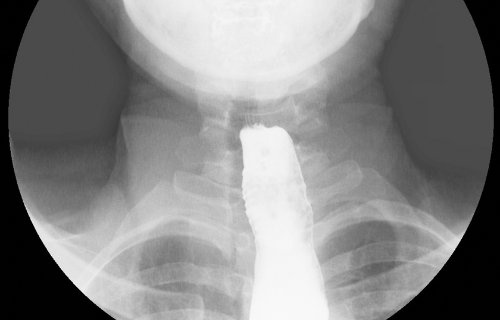
Diagnostic tools for achalasia most commonly used are barium studies where patient swallow a fluid which appears on radiographic studies. During barium studies, patients with primary achalasia present with a smooth and even narrowing of the lower oesophagus of less than 3,5cm. There is also a clinical presentation of a delayed stomach emptying.
Other diagnostic tests done include an amyl nitrite test where patients inhale a smooth muscle relaxant which should relax the sphincter muscle in the stomach. Patients suffering achalasia have a relaxing response of about 2mm.
Endoscopy is a procedure often done, where a tubed camera passes into the stomach, to identify achalasia. Finally, a CT scan is done as an imaging technique to diagnose achalasia.
Pseudoachalasia
Barium swallow studies are also the diagnostic tool of choice for pseudoachalasia. During barium studies patients present with a smooth and even narrowing of the lower oesophagus. However, the narrowing is over a longer section than in the case of primary achalasia and seen to be greater than 3,5cm.
When pseudoachalasia is present, there is no relaxation of the stomach sphincter during an amyl nitrite test. Endoscopy is also often attempted, but in pseudoachalasia the scoping apparatus is unable to pass into the stomach.
Finally, a CT scan may show the presence of a lesion at the junction where the oesophagus joins the stomach.
Symptoms
Achalasia
Symptoms described by patients suffering achalasia often include:
- The sensation of having a difficult time swallowing
- Reflux or food coming back up after it has been swallowed
- Heart burn sensation and a feeling of pain in the chest
- Generalized weight loss
Pseudoachalasia
Symptoms presenting in patients suffering from pseudoachalasia most often include:
- A significant weight loss over a short term
- Worsening difficulty swallowing
- Chest pain
- Regurgitation of food after it has been swallowed
Treatment
Achalasia
Achalasia is treated by focusing on relaxing the lower part of the oesophagus through medications. Surgical stretching of the lower oesophagus is also often done by specialist surgeons. This will allow the food or liquid to travel through the digestive passage with ease.
The surgical procedures include pneumatic dilation – where a balloon is placed through the oesophagus and inflated to stretch the affected area. Botox can be injected into the oesophageal sphincter muscle directly to relax and paralyze it.
The majority of patients who are correctly treated can live a relatively normal life. Unfortunately, the disease has a tendency to occur again but can be treated just as effectively.
Pseudoachalasia
Due to the fact that pseudoachalasia being associated with an obstruction or blockage at the point where the stomach and oesophagus meet, treatment is mostly to remove it. The obstructions are usually malignant and require treatment with chemotherapy or radiation therapy sessions.
The surgical procedures to remove these malignancies include esophagogastrostomy or a subtotal McKeown esophagectomy.
In severely advanced cases, palliative care is recommended.
Table of comparison between
Summary
Although similar in symptoms and diagnosis, achalasia and pseudoachalasia are two very different cases. Achalasia has no known cause, where pseudoachalasia is most often caused by malignant or benign tumours. Achalasia is usually treated with medications, pneumatic dilation or botox injections. Pseudoachalasia, however, requires the obstruction to be surgically removed and is often coupled with intensive therapies.
FAQ
How is Pseudoachalasia different from achalasia?
Pseudoachalasia is a secondary state of achalasia and is usually caused by a malignancy, where achalasia is a primary condition and of unknown causes.
What is the difference between achalasia and dysphagia?
Achalasia is a diagnosed condition and dysphagia is a common symptom of that condition.
What is Pseudoachalasia?
Pseudoachalasia is a type of secondary achalasia that most often occurs in adults over the age of 50 years old. It is defined as a secondary achalasia caused by malignant tumours or by a chronic medical disease.
What causes Pseudoachalasia?
Pseudoachalasia is most often caused by malignancies, benign tumours, or chronic medical conditions.
- Difference Between a Cochlear Implant and Normal Hearing - October 4, 2022
- Difference Between Obstructive and Restrictive Spirometry - September 11, 2022
- The Difference Between White Box and Black Box Testing - September 11, 2022
Search DifferenceBetween.net :
Leave a Response
References :
[0]Abubakar, U., Bashir, M. & Kesieme, E. “Pseudoachalasia: A review”. Nigerian Journal of Clinical Practice, vol. 19, no. 3, 2016, pp: 303-307.
[1]Di Lorenzo, C. & Youssef, N. “Diagnosis and management of intestinal motility disorders”. Seminar of Paediatric Surgery, vol. 19, no. 1, 2010, pp: 50-58.
[2]Gyawali, C. “Achalasia: new perspectives on an old disease”. Neurogastroenterological Motility, vol. 28, no. 1, 2016, pp:4-11.
