Difference Between Pericarditis and Myocardial Infarction
Both pericarditis and myocardial infarction involve chest pain, palpitations, and shortness of breath. Pericarditis is the inflammation of the pericardium while myocardial infarction occurs when one or more areas of the heart muscle do not have enough oxygen due to blocked blood flow to the heart muscle. The following discussions further delve into their differences.
What is Pericarditis?
Pericarditis (“peri-” for “surrounding”; “kardia” for “heart”; “-itis” for “inflammation”) is the inflammation of any of the layers of the thin tissue sac (the pericardium) surrounding the heart (Beckerman, 2020).
Symptoms:
The symptoms include sharp chest pain (center or left side), heart palpitations, shortness of breath, fatigue, abdominal swelling, leg swelling, nausea, and low fever (Health Direct, 2021).
Causes:
The causes of pericarditis include viral infection (the most common), autoimmune disorders (specially for recurring pericarditis), myocardial infarction, cancer, acquired immune deficiency syndrome, kidney failure, and drug (i.e., warfarin and heparin) side effects (American Heart Association, 2022)
Treatment:
A number of patients with pericarditis recover in around two to four weeks (Beckerman, 2020). The treatments for pericarditis include taking antibiotics, taking non-steroidal anti-inflammatory drugs (NSAIDs), refraining from engaging in strenuous activities, and undergoing surgery (American Heart Association, 2022).

What is Myocardial Infarction?
Myocardial infarction (“myo” means muscle; “cardial” pertains to the heart; “infarction” means tissue death due to lack of blood supply) is also known as heart attack; it occurs when one or more areas of the heart muscle do not have enough oxygen due to blocked blood flow (Johns Hopkins Medicine, 2022).
Symptoms:
The symptoms for myocardial infarction include the following (Beckerman, 2020):
- discomfort (i.e., pressure, squeezing, or heaviness) or pain in the chest, arm, or below the breastbone
- discomfort which goes into the jaw, throat, arm, or back
- a feeling of fullness, choking, or indigestion
- upset stomach, vomiting, dizziness, or sweating
- fatigue, shortness of breath, or anxiety
- palpitations or uneven heartbeat
Some people (more common in those who have diabetes) experience silent heart attacks, they do not notice any symptoms.
Causes/ Risk Factors
The blocked blood flow is due to the buildup of plaque (made up of cholesterol, deposits, and other substances) in the arteries. The actual cause of myocardial infarction is the blood clot which is quickly formed when a plaque breaks. Irreversible damage begins within 30 minutes of blocked oxygen and blood supply to the heart.
Regarding genetic factors, those who are at risk include those who have inherited high blood pressure, low levels of HDL cholesterol, high levels of LDL cholesterol, or high levels of triglycerides; also, those with a family history of heart disease, people with type 1 diabetes, and the elderly. As for those with acquired risk factors, the groups that are most at risk are those with acquired hypertension, people who acquired low levels of HDL cholesterol, high levels of LDL cholesterol, or high levels of triglycerides, smokers, those who consume too much alcohol, individuals with sedentary lifestyles, and people with type 2 diabetes (Johns Hopkins Medicine, 2022).
Treatment:
Since myocardial infarction is a medical emergency, the treatment starts in the ambulance or in the emergency room. Medications such as aspirin and other antiplatelets and anticoagulants are given to limit heart damage. Procedures to open the blocked arteries include cardiac catheterization, balloon angioplasty, and stent replacement. After the critical phase, various drugs are given such as beta-blockers, nitrates, blood thinners, ACE inhibitors, and statins. A patient may have bypass surgery to restore blood supply to the heart. For some patients, they are fitted with pacemakers to help keep a steady heart rhythm (Beckerman, 2020).
Difference between Pericarditis and Myocardial Infarction
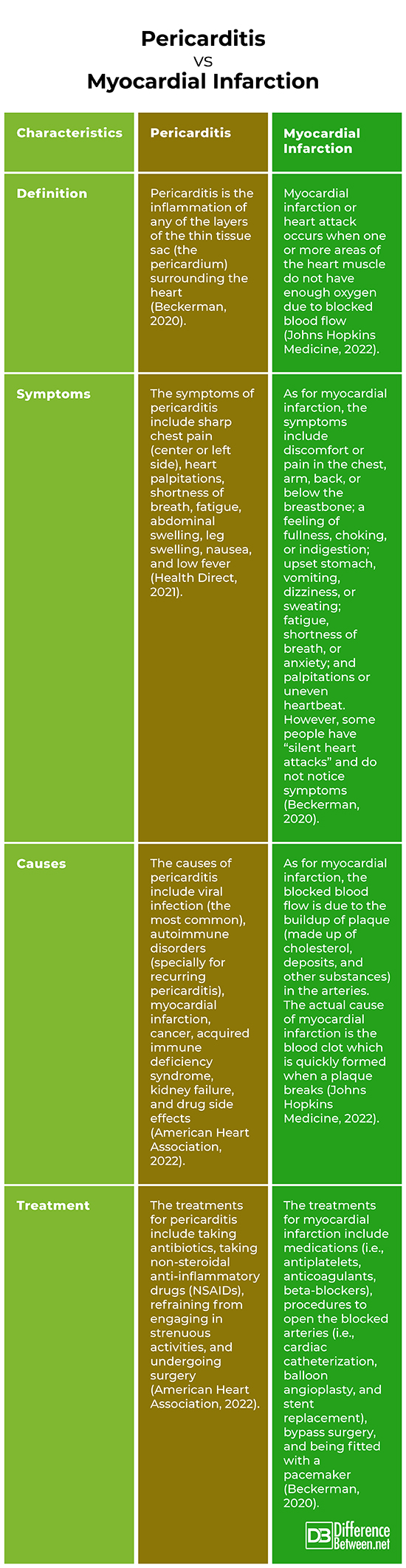
Definition
Pericarditis is the inflammation of any of the layers of the thin tissue sac (the pericardium) surrounding the heart (Beckerman, 2020). In comparison, myocardial infarction or heart attack occurs when one or more areas of the heart muscle do not have enough oxygen due to blocked blood flow (Johns Hopkins Medicine, 2022).
Symptoms
The symptoms of pericarditis include sharp chest pain (center or left side), heart palpitations, shortness of breath, fatigue, abdominal swelling, leg swelling, nausea, and low fever (Health Direct, 2021). As for myocardial infarction, the symptoms include discomfort or pain in the chest, arm, back, or below the breastbone; a feeling of fullness, choking, or indigestion; upset stomach, vomiting, dizziness, or sweating; fatigue, shortness of breath, or anxiety; and palpitations or uneven heartbeat. However, some people have “silent heart attacks” and do not notice symptoms (Beckerman, 2020).
Causes
The causes of pericarditis include viral infection (the most common), autoimmune disorders (specially for recurring pericarditis), myocardial infarction, cancer, acquired immune deficiency syndrome, kidney failure, and drug side effects (American Heart Association, 2022). As for myocardial infarction, the blocked blood flow is due to the buildup of plaque (made up of cholesterol, deposits, and other substances) in the arteries. The actual cause of myocardial infarction is the blood clot which is quickly formed when a plaque breaks (Johns Hopkins Medicine, 2022).
Treatment
The treatments for pericarditis include taking antibiotics, taking non-steroidal anti-inflammatory drugs (NSAIDs), refraining from engaging in strenuous activities, and undergoing surgery (American Heart Association, 2021). In comparison, the treatments for myocardial infarction include medications (i.e., antiplatelets, anticoagulants, beta-blockers), procedures to open the blocked arteries (i.e, cardiac catheterization, balloon angioplasty, and stent replacement), bypass surgery, and being fitted with a pacemaker (Beckerman, 2020).
Pericarditis vs Myocardial Infarction
Frequently Asked Questions (FAQs):
Can pericarditis cause myocardial infarction?
Myocardial infarction can cause pericarditis; the inflammation of the pericardium may occur days, weeks, or months after a heart attack (Bennington-Castro, 2020).
Which is worse pericarditis or myocarditis?
Myocarditis is associated with more long-term after-effects than pericarditis. The most serious effects are dilated cardiomyopathy and heart failure (Sharif & Dehghani, 2013).
Is pericarditis a heart attack?
Though a common symptom of pericarditis is chest pain, it is not a heart attack. The chest pain may be due to the inflamed pericardium’s rubbing against the heart (American Heart Association, 2022).
What can pericarditis be mistaken for?
Pericarditis may be mistaken for a heart attack due to the chest pain. If you feel chest pain, it is best to call 911 because you may be having a heart attack (American Heart Association, 2022).
Summary
- Pericarditis is the inflammation of any of the layers of the thin tissue sac (the pericardium) surrounding the heart.
- Myocardial infarction or heart attack occurs when one or more areas of the heart muscle do not have enough oxygen due to blocked blood flow to the heart muscle.
- The symptoms of pericarditis include sharp chest pain, heart palpitations, shortness of breath, fatigue, abdominal and leg swelling, nausea, and low fever.
- The symptoms for myocardial infarction include discomfort or pain in the chest, arm, back, or below the breastbone; a feeling of fullness, choking, or indigestion; upset stomach, vomiting, dizziness, or sweating; fatigue, shortness of breath, or anxiety; and palpitations.
- Difference Between Hematoma and Melanoma - February 9, 2023
- Difference Between Bruising and Necrosis - February 8, 2023
- Difference Between Brain Hematoma and Brain Hemorrhage - February 8, 2023
Search DifferenceBetween.net :
Leave a Response
References :
[0]American Heart Association (2022). What is pericarditis. https://www.heart.org/en/health-topics/pericarditis/what-is-pericarditis
[1]Beckerman, J. (2020). Heart attack. WebMD. https://www.webmd.com/heart-disease/guide/heart-disease-heart-attacks
[2]Beckerman, J. (2020). Heart disease and pericarditis. WebMD. https://www.webmd.com/heart-disease/guide/heart-disease-pericardial-disease-percarditis
[3]Bennington-Castro, J. (2020). What is pericarditis? Everyday Health. https://www.everydayhealth.com/pericarditis/guide/
[4]Burns, E. & Buttner, R. (2021). Pericarditis. Life in the Fast Lane. https://litfl.com/pericarditis-ecg-library/
[5]Health Direct (2021). Pericarditis. https://www.healthdirect.gov.au/pericarditis
[6]Johns Hopkins Medicine (2022). Heart attack. https://www.hopkinsmedicine.org/health/conditions-and-diseases/heart-attack#:~:text=A%20heart%20attack%20(myocardial%20infarction,the%20heart%20muscle%20is%20blocked.
[7]Marinella, M. (1998). Electrocardiographic manifestations and differential diagnosis of acute pericarditis. American Family Physician. https://www.aafp.org/afp/1998/0215/p699.html
[8]Sharif, N. & Dehghani, P. (2013). Acute pericarditis, myocarditis, and worse! Canadian Family Physician. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3555652/
[9]Teh, B.S., Walsh, J., Bell, A.J., Walker, S.J., & Kilpatrick, D. (1993). Electrical current paths in acute pericarditis. PubMed. https://pubmed.ncbi.nlm.nih.gov/8228718/
[10]UpToDate (2022). Patient education: Pericarditis (Beyond the Basics). https://www.uptodate.com/contents/pericarditis-beyond-the-basics
[11]Wedro, B. (2021). Pericarditis. MedicineNet. https://www.medicinenet.com/pericarditis/article.htm
