Difference Between Actinic Keratosis and Eczema
What is actinic keratosis and eczema?
Actinic keratosis aka Solar keratosis is the most common premalignancy condition that forms on skin due to the damage caused by the lifelong and chronic exposure to harmful UV rays from the sun and/or indoor tanning.
Eczema is a most common inflammatory disease that develops in early childhood and is a genetic problem. The most common symptom is a rash followed by dryness, redness and itching. It typically appears on the arms, neck, hands and behind the knees, but can also appear anywhere.
Similarity
Both are conditions of the skin.

Actinic keratosis
A rough, scaly spot that is a precancerous condition on the skin caused by years of sun exposure.

Eczema
Eczema is an inflammatory skin disease that involves patches of dry itchy skin. It develops in the form of rash behind the knees, arms, hands and neck. The rash eventually turns red and dry.
Difference between actinic keratosis and eczema
Description
Actinic keratosis is an irregular or scaly skin growth or spot that usually develop on sun-damaged skin. This skin condition usually develops on hands, face, neck, arms, and shoulder. It is also termed as solar keratosis. While actinic keratosis is harmless, a minute percentage of these lesions (about 10 percent) develop into skin cancer, specifically cutaneous squamous cell carcinoma (a keratinocyte cancer).
Eczema
Eczema is a condition that is also termed as itch that rashes. It’s common in children but can happen to adults as well. It causes inflammation that is chronic and relapsing.
Symptoms
Actinic keratosis
Some of the common symptoms shown by people who develop actinic keratosis include;
- Scaly, patched, thickened and rough skin. These skin patches (usually less than 1 inch (2.5 centimeters) in diameter) are often termed as plaques
- Clusters of plaques in the same region
- Growths may appear and vanish in the same area
- A hard, bumpy wartlike surface in some cases
- Tender or asymptomatic
- Poorly marginated, slightly raised or flat lesions
- Lesions usually vary inconsistently in shade tone like yellowish, brownish, skin colored or black to blotchy
- Lesions bleed on touching. They even change in shape, texture and color. The sores developed due to this condition takes a longer duration of time to heal
- It is common on sites that are exposed to the sun light repeatedly, nose, ears, upper lip, vermillion of the lower lip, forehead, temples, back of the hands, cheeks, and the balding scalp.
- In rare cases, affected areas may show symptoms like burning sensation, itching, or cause other unpleasant or uncomfortable sensations
Eczema
Some of the common symptoms shown by people who develop eczema include;
- Red, inflamed or swollen skin
- Tiny fluid-filled blisters (vesicles)
- Dry, easily irritated skin
- Intense itching – more in people with eczema and possibility of infections to develop
- Patches of dark skin
- Leathery crusts or scabs that form when the fluid dries
- Scaly patches of skin (lichenified skin)
- Itchy red patches on the legs
- Itchy forearms
- Red raised bumps due to excess blood flowing through the blood vessels on the inner elbow
Causes
Actinic keratosis
The main cause of actinic keratosis is sun’s UV (ultraviolet) exposure. This is the reason this condition is often termed as solar keratosis. There is an increased risk of developing Actinic keratosis if you;
- Are above 60 years of age
- Possess light skin tone and blue eyes
- Possess a tendency to easily sunburn
- Have been exposed to sunlight over lifetime
- Are suffering from HPV (Human Papilloma Virus)
- Possess a history of sunburns (genetics)
Eczema
- Hereditary factors (genetics) – eczema runs in families
- Immune system dysfunction resulting in an undesired inflammatory response in the skin
- Irritants and allergens like pollen, certain foods, wool, excess heat, moulds, dust mites, soaps and detergents, skin infections, reduced humidity, sweating or mental stress.
Treatment
Actinic keratosis
- Excision
- Cauterization – the lesion or the affected area is burnt and cells killed using electric current
- Cryotherapy – the lesion or the affected area of the skin is sprayed with a cryosurgery solution (liquid nitrogen). The cells get frozen and destructed. The lesion will scab over and get removed in some days after the cryotherapy.
- Topical medical therapy – ingenol mebutate (Picato), 5-fluorouracil and imiquimod (Aldara, Zyclara) cause inflammation and destruction of the lesions.
- Phototherapy – a medical solution is applied over the affected area of the skin. Then intense laser light is used over the lesion that kills the cells.
Eczema
Some very mild cases of condition like eczema can be managed by:
- Avoiding irritants or certain factors (allergens) that could flare up the condition
- Using emollients like bath oils and moisturisers.
Medications
- Corticosteroid creams and ointments available on prescription.
- Pimecrolimus cream (Elidel) – a steroid-free medication
- Antihistamines may help the itching
- Antibiotics in the form of syrup, capsules, or tablets.
Other therapies include Phototherapy, or ultraviolet (UV) light treatment which involves controlled exposure to sun’s ultraviolet rays
Summary
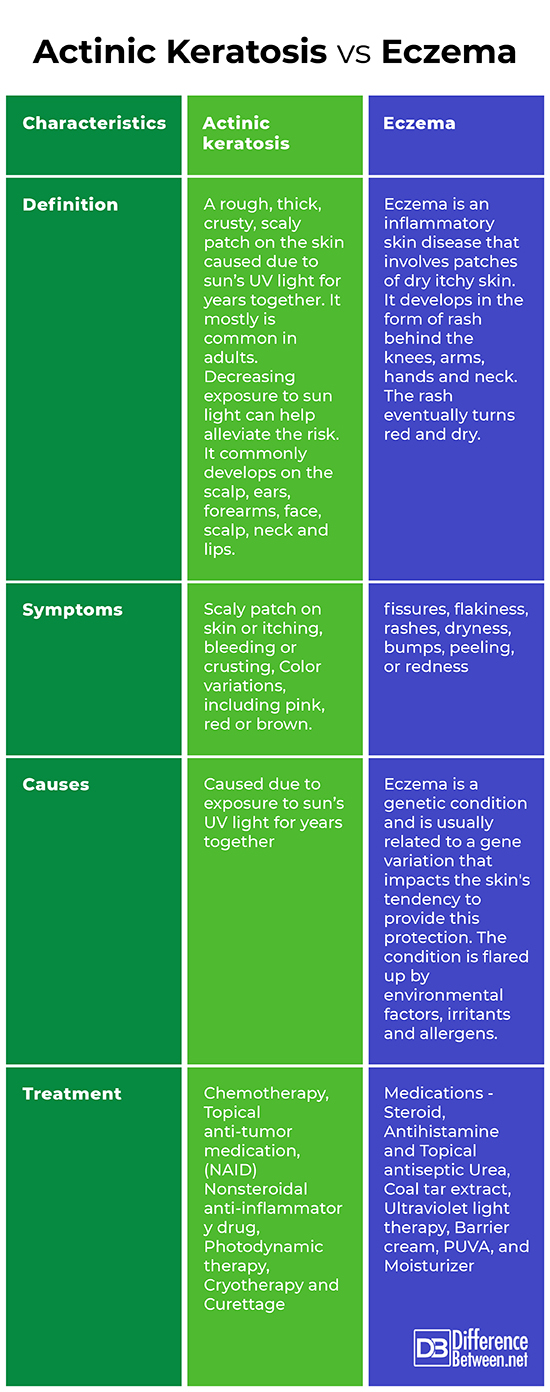
The points of difference between Actinic keratosis and Eczema have been summarized as below:
Actinic keratosis Vs. Eczema
- Difference Between Global Warming and Greenhouse Effect - May 18, 2024
- Difference Between Vaccination and Immunization - March 3, 2024
- Difference Between Selective Mutism and Autism - February 25, 2024
Search DifferenceBetween.net :
Leave a Response
References :
[0]Diepgen, T. L., Agner, T., Aberer, W., Berth‐Jones, J., Cambazard, F., Elsner, P., ... & Coenraads, P. J. (2007). Management of chronic hand eczema. Contact dermatitis, 57(4), 203-210.
[1]Hoare, C., Po, A. L. W., & Williams, H. (2000). Systematic review of treatments for atopic eczema. Health technology assessment (Winchester, England), 4(37), 1.
[2]Jeffes, E. W., & Tang, E. H. (2000). Actinic keratosis. American journal of clinical dermatology, 1(3), 167-179.
[3]Siegel, J. A., Korgavkar, K., & Weinstock, M. A. (2017). Current perspective on actinic keratosis: a review. British Journal of Dermatology, 177(2), 350-358.
[4]Image credit: https://live.staticflickr.com/3061/2703075480_8aa728fa6b_b.jpg
[5]Image credit:https://commons.wikimedia.org/wiki/File:Actinic_keratoses_on_forehead.JPG
